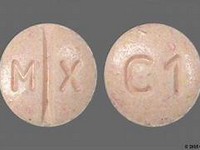
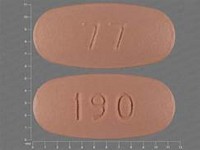
oxybutynin hydrochloride

CLINICAL USE
Urinary frequency, urgency and incontinenceNeurogenic bladder instability and nocturnal enuresisDOSE IN NORMAL RENAL FUNCTION
2.5–5 mg 2 to 3 times a day; maximum 5 mg 4 times a dayXL: 5–20 mg once daily Patches: 1 patch (36 mg) twice weeklyPHARMACOKINETICS
DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugsOther antimuscarinic agents: increased antimuscarinic effectsADMINISTRATION
Reconstition
–Route
Oral, topicalRate of Administration
–Comments
–OTHER INFORMATION
Start with a low dose in elderly patients and those with renal impairment, and increase according to response
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home